Sleep Apnea, or Just Snoring?
Sleep apnea, or just snoring? Nowadays, the incidence of shortness of breath during sleep among individuals is increasingly common.
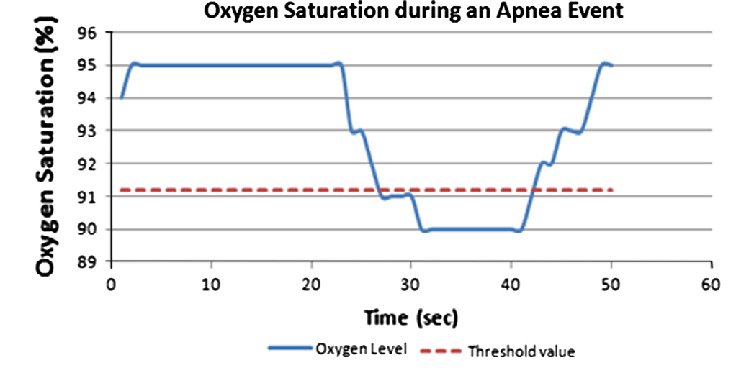
Sleep apnea is not just snoring. It stops being snoring and becomes apnea when there are noises and interruptions in breathing that are repeated, at least, five times in a period of 60 minutes. The person has breathing difficulty during the night, stops breathing, and may even choke without realizing it. And what happens when you stop breathing? The brain does not oxygenate properly (hypoxemia – lack of oxygen in the blood; hypercapnia – increased carbon dioxide), affecting the nervous system, increasing the heartbeat rhythm, and causing contract of blood vessels – being, therefore, considered as a risk factor for high blood pressure and cardiac arrhythmia. Although patients can sleep, the brain does not rest.
Signals and symptoms
- Snoring, wheezing
- Restless sleep, insomnia
- Drowsiness throughout the day, difficulty concentrating
- Greater irritability
- Headaches
- Sexual dysfunctions
Risk factors
- Nasal congestion / Allergic rhinitis
- Overweight (fat deposits in the structures surrounding the pharynx and tongue, reducing the space for air to pass)
- Smaller lower jaw (pushes back the tongue and can cover the throat)
- Smoking (inflammation of the upper airways and can also interfere with the brain mechanisms involved in breathing)
- Alcoholism (increases the relaxation of the muscles of the mouth and throat and can also interfere with the control of the brain over the muscles involved in breathing)
- Misuse of sedatives
- Enlarged tonsils or adenoids
- Sleeping on your back
- Age (with aging, the tissues of the oropharynx tend to become flabbier, facilitating obstructions, so the risk increases among individuals over 65)
In addition to these symptoms and factors, some conditions can be aggravated due to disturbed sleep apnea. Depression and anxiety, both disorders that condition the individual’s life and are still the target of some disabling stigma, can appear or become more serious, due to the lack of hours of sleep and the lack of quality of sleep day after day.
As we can see, it is a disturbance that can condition many aspects of people’s lives. So, how can we deal with this problem?
Sleep Apnea Treatment
The first step of sleep apnea treatment is its diagnosis – it is usually identified by the partners. To assess suspected sleep apnea, the doctor (pulmonologist) asks about the quality of sleep, complaints about snoring, and daytime tiredness, in addition to examining the circumference of the neck, the inside of the nose, and the jaws. Confirmation and analysis of disorder severity are done through an exam called polysomnography – performed in a sleep laboratory at the hospital or specialized clinic – where the patient spends the night connected to a device that records heartbeat, brain activity, eye movement, breathing, and oxygen level in the blood. This examination will also allow you to evaluate the effectiveness of subsequent treatment in the future.
Depending on the test result, the disorder can be classified as:
- Light: from five to 14 apneas per hour;
- Moderate: 15 to 29 apneas per hour;
- Severe: 30 or more apneas per hour.
Other tests may be ordered to investigate the causes or complications of the problem, such as radiographs, dentist evaluations, or blood tests.
Polysomnography uses the following terms:
Apnea: decrease greater than 90% of the airflow amplitude lasting 10 seconds or more.
Hypopnea: reduction of more than 30% in airflow amplitude, accompanied by a decrease in oxygen saturation equal to or greater than 3% and/or micro-awakening, for at least 10 seconds.
RERA (RESPIRATORY EFFORT-RELATED AROUSAL): flattening of the nasal flow curve or increased respiratory effort that precedes awakening (without fulfilling apnea or hypopnea criteria).
Apnea / Hypopnea Index (AHI): number of apneas and hypopneas per hour of recording.
RDI (Respiratory Disturbance Index): is the number of apneas, hypopneas, and RERAs per hour of sleep.
This disorder treatment includes general measures and, depending on each case, a specific intervention. The general measures, in the mildest cases, can be weight reduction; do not drink alcohol after lunch; do not smoke; not taking sleeping pills; enough hours of sleeping (at least seven hours). Therapy with a speech therapist can be used: specific exercises to strengthen the muscles that involve the tongue, pharynx, and face can bring good results for some cases of snoring and apnea. The patient must create a sleep routine, only associating bed with sleep, and if he cannot sleep for some reason, he must get up and perform activities until he is asleep. You should sleep in the lateral position and have a regular time to sleep.
In more severe cases, measures such as the use of braces in the mouth or masks that facilitate sleep breathing are necessary. CPAP (Continuous Positive Airway Pressure) is considered the standard treatment for moderate to severe sleep apnea. The equipment keeps the airway unobstructed through the constant passage of air at a certain pressure, with a mask (usually nasal) that must be adapted to the patient’s face shape. Intraoral, orthodontic, or dental devices can be used – they help to reposition the lower jaw to keep the airways clear during the night – recommended as an alternative therapy for patients who refuse to use CPAP and who have mild to moderate apnea.
Some patients may still need surgery, in cases of anatomical obstruction that can occur when there is tonsil or adenoid hypertrophy or craniofacial anomalies.
And still…
Why is sleep apnea a social problem?
- Higher risk of accidents: about 7 times higher than that of the general population;
- Higher consumption of health resources: namely, a higher number of consultations, hospitalizations, and medications;
- Possible marital and family problems: due to snoring, mood changes, and sexual disorders;
- Decreased productivity.
How to help apnea sufferers?
Family members play an important role in the apnea diagnosis and treatment because treatment requires changes in habits, which is not easy. Dieting and exercise are always easier when the whole family participates. Treatment can also involve routines that require adaptation, especially at the beginning, such as sleeping in the laboratory a few times, using the devices every night, and taking care of their maintenance is easier when there is support from someone.
After starting treatments, how long does it take to notice any improvement?
Some people notice an improvement immediately after starting CPAP therapy. Others do not notice a significant difference. The most important factor is that apnea is being treated and you are eliminating the negative effects that it has on your body. Normally, you will not snore with the use of your CPAP mask. If your symptoms persist, you should see your doctor.
Why do I need follow-up?
Apnea is a chronic condition. If it does not get better with the CPAP treatment, which deals only with the symptoms so that you can get adequate rest and supply the oxygen that your body needs every night. When you realize the benefits of CPAP therapy, you may want to stop using your mask and equipment, as you will be feeling healed. But not quite. As with any chronic condition, you benefit from continuous assessment, with proper training and product guidance, which will help you enjoy the better health and quality of life that are provided by long-term CPAP therapy.
Sleep apnea is well known, there are already several forms of monitoring and treatment. It can be a long process, but it is not complicated. Help yourself, to have a better quality of life.
You may also like; Types of sleep.
Al-Mardini, M., Aloul, F., Sagahyroon, A., & Al-Husseini, L. (2014). Classifying obstructive sleep apnea using smartphones. Journal of biomedical informatics, 52, 251-259.
Kanchanawong, P. & Waterman, C., (2020). NATIONAL HEART, LUNG, AND BLOOD INSTITUTE [Online]. Available at: https://www.nhlbi.nih.gov/ (accessed April 10th, 2021).
N.D. (2021). Medline Plus. Trusted health information for you [Online]. Available at: https://medlineplus.gov/ (accessed April 10th, 2021).